Can U.S. Health Care Escape MACRA's Bureaucratic Briar Patch?

Congress has struggled for decades to reform Medicare’s fee-for-service payment system, which has driven up the cost of American health care by reimbursing medical providers for services, regardless of their value or quality. The most recent attempt at reform, the 2015 Medicare and CHIP Reauthorization Act (MACRA), seeks to quantify the value of care delivered and to get medical practices to bear some responsibility for the aggregate costs associated with a course of treatment.
To do so, the law provides higher payments to clinicians who participate in Alternative Payment Models (APMs), in which practices are penalized for excessive aggregate costs associated with the delivery of a full course of treatment. Most medical practices have balked at APMs, which require them to bear substantial financial risks. These practices, however, will become subject to a complex grading mechanism, the Merit-based Incentive Payment System (MIPS), which will adjust Medicare payments to clinicians in line with their performance relative to peers on a vast array of performance metrics. Yet the federal agency tasked with overseeing this scoring system has publicly declared MIPS to be unworkable and called for its repeal.
The fact that Medicare has inadvertently encouraged the proliferation of low-value services does not mean that it is capable of transforming health care for good by identifying and rewarding high-value care. It would be enough to avoid doing harm. That goal can be accomplished if APMs were to give clinicians full credit for treating patients enrolled in Medicare Advantage—which would eliminate the risk to taxpayers of inflated volumes of low-value services, while freeing medical practitioners from arbitrary and counterproductive regulations.
______________________
Chris Pope is a senior fellow at the Manhattan Institute. Follow him on Twitter here.
Executive Summary
Congress has struggled for decades to reform Medicare’s fee-for-service payment system, which has driven up the cost of American health care by reimbursing medical providers for services, regardless of their value or quality. The most recent attempt at reform, the 2015 Medicare and CHIP Reauthorization Act (MACRA), seeks to quantify the value of care delivered and to get medical practices to bear some responsibility for the aggregate costs associated with a course of treatment.
To do so, the law provides higher payments to clinicians who participate in Alternative Payment Models (APMs), in which practices are penalized for excessive aggregate costs associated with the delivery of a full course of treatment. Most medical practices have balked at APMs, which require them to bear substantial financial risks. These practices, however, will become subject to a complex grading mechanism, the Merit-based Incentive Payment System (MIPS), which will adjust Medicare payments to clinicians in line with their performance relative to peers on a vast array of performance metrics. Yet the federal agency tasked with overseeing this scoring system has publicly declared MIPS to be unworkable and called for its repeal.
The fact that Medicare has inadvertently encouraged the proliferation of low-value services does not mean that it is capable of transforming health care for good by identifying and rewarding high-value care. It would be enough to avoid doing harm. That goal can be accomplished if APMs were to give clinicians full credit for treating patients enrolled in Medicare Advantage—which would eliminate the risk to taxpayers of inflated volumes of low-value services, while freeing medical practitioners from arbitrary and counterproductive regulations.
Introduction
Medicare costs have risen dramatically over recent decades—from $8 billion in 1970 to $679 billion in 2017. Since the 1980s, Congress has gradually fixed fees for hospital and physician services, slowing their growth. But this effort at cost control inadvertently encouraged providers to increase the number of consultations and services for which they claim separate reimbursement.
In response, Congress in 1997 enacted a mechanism to automatically reduce Medicare physician fees when aggregate national spending exceeded a Sustainable Growth Rate (SGR). But the SGR device was flawed. It reduced fees equally for low-billing and high-billing clinicians—failing to constrain spending by providers responsible for inflating volumes while threatening the solvency of those whose revenues were slim. As a result, SGR cuts were overridden 17 times by Congress before being repealed.
In 2015, Congress passed the Medicare and CHIP Reauthorization Act (MACRA), with broad bipartisan support. MACRA has two core goals: replacing SGR’s failed method of fixing Medicare’s volume problem; and using the Medicare program to reduce the provision of low-value care across America’s health-care delivery system more generally.
The new law sought to do this by establishing Alternative Payment Models (APMs), which adjust Medicare payments to clinicians in accordance with the aggregate costs incurred by a patient during a full course of treatment. The objective is to get clinicians to focus on patient outcomes, to reward them for cost-effective preventive care, and to discourage them from incurring unnecessary expense. Yet in 2017, only 7% of clinicians chose to receive payment through APMs—and most medical practices have balked at a change that may penalize them for patients’ use of services over which they have no control.
But MACRA requires non-APM participants to comply with a regulatory protocol known as the Merit-based Incentive Payment System (MIPS)—a stunningly complex system that adjusts Medicare reimbursement rates according to clinicians’ self-reported performance relative to peers on a vast number of metrics loosely associated with cost, quality, computerization, and participation in federal health initiatives. MedPAC (Medicare Payment Advisory Commission), the agency established by Congress to advise it on Medicare payment policy, has declared MIPS to be unworkable and called for it to be repealed. The agency has argued that, by imposing an enormous array of clinical process metrics that tend to be poorly correlated with medical outcomes and skewed by variation in patient characteristics, MIPS is unlikely to be able to identify or reward high-value care.
In short, physicians lack the interest or ability to engage in meaningful APMs, while MIPS threatens to drown them in paperwork and arbitrary and futile bureaucratic interference.
Medicare bears much of the responsibility for inflating the volume of low-value services provided by hospitals and physicians. But any attempt to reconstruct the care coordination and cost-control advantages of managed care within Medicare’s open-network fee-for-service benefit structure is fundamentally flawed. Medicare patients will not limit themselves to medical practices that decline to furnish low-value care from them unless they see some benefits from the savings.
Medicare Advantage (MA) provides the benefits and relieves the Medicare program of the arduous task of reforming fee-for-service reimbursement. In MA plans, the Medicare program pays insurers or integrated medical systems a single fee, adjusted according to enrollees’ expected medical needs, to deliver all medical care to which Medicare beneficiaries are entitled. Plans, therefore, have a strong incentive to identify and eliminate low-value care, as they are able to use the savings to attract enrollees by cutting premiums, reducing cost-sharing, and providing supplemental benefits such as dental care or prescription drug coverage with no additional premiums. MA payment arrangements, without imposing arbitrary and counterproductive regulatory standards on clinicians, entirely protect taxpayers from incentives to inflate volumes of low-value care—even in the case of private fee-for-service MA plans, which lack any of the characteristic features of managed care. Medical practices ought therefore to be able to count their patients’ participation in any MA plan, regardless of its internal structure, toward the bonus they receive for participation in risk-bearing APMs under MACRA.
A Short History of Medicare Payments
Medicare serves 57 million elderly and disabled Americans and dominates the purchase of most medical services in the United States. The cost of the entitlement has risen from $8 billion in 1970 to $679 billion in 2017—the result of increased prices for services, the development of new medical procedures, increased rates of utilization, an expanded benefits package, and people living longer.[1]
To secure the support of hospitals and doctors for the launch of the Medicare program, Congress originally promised to pay them according to what they claimed it cost to treat eligible beneficiaries. This led to physicians billing the government up to four times what they billed private insurers to treat patients; it also created an incentive for hospitals to inflate the cost of delivering care.[2]
Between 1967 and 1983, Medicare spending on hospitals soared from $3 billion to $37 billion, as hospitals competed by making enormous capital investments in cutting-edge technology and facilities proliferated with little regard for efficient levels of equipment, staffing, and occupancy. This drove up health-care costs for those not enrolled in Medicare.[3]
Over the past few decades, policymakers have struggled to rein in the program’s spending. In 1983, Congress established fixed payment amounts for hospitals treating inpatients with specific medical diagnoses (Diagnosis Related Groups, or DRGs), encouraging Medicare beneficiaries to shop around for the best treatment at the given price.[4]
This proved very successful at controlling costs without adversely affecting quality or access to care, and slowed the increase of hospital spending from an average of 14% per year between 1965 and 1982 to an average of 6% since then.[5]
Physician services, payments to anesthesiologists, and follow-up care were not included in DRG payments. Thus, while the growth of hospital costs slowed during the 1980s, Medicare spending on other services picked up speed.[6] To extend the cost-control effort to physician services, Congress in 1992 enacted a complex formula to generate a Physician Fee Schedule for 10,000 medical procedures, according to an expert panel’s determination of the physician qualifications, time, and effort involved.[7] Additional reimbursements were provided for the use of laboratory tests, scans, medical devices, and physician-administered drugs.
Congress sought to constrain the growth of spending on physician services by enacting an automatic adjustment of reimbursement rates, which would raise or lower fees as needed to keep aggregate spending on medical services in line with a target growth rate. But this led to hikes in reimbursements when the growth rate of spending slowed—and unsustainable cuts when it rose.[8] The target was switched in 1999 from a Volume Performance Standard (based on per-capita economic growth) to a Sustainable Growth Rate, or SGR (incorporating historical cost growth rates). But the flawed mechanism remained essentially the same: reducing rates for all physicians equally—those who kept the volume of services they billed Medicare at the same level as before, just as much as those responsible for inflated volumes—so this system did little to slow the rapid growth of costs.
Indeed, the SGR mechanism had major unintended consequences: it inflated the disparity in incomes between primary care physicians and specialists. The SGR also encouraged physicians to affiliate with hospitals, which received higher reimbursements (in 2011, Medicare paid an average of $212 for an electrocardiogram in a hospital, compared with only $37 in a physician’s office).[9] While Medicare physician fees increased by 10% from 2000 to 2015, physician service spending per beneficiary increased by 71%.[10]
As overall Medicare spending continued to increase, the cuts in fees needed to meet the SGR became unsustainably large (21% in 2015). With many primary care physicians threatening to stop accepting Medicare patients, medical lobbyists were able to get these cuts overturned 17 times through annual legislative patches known as the “Doc Fix.”[11] By 2015, Congress had grown tired of finding money to patch physician fees every year, and enacted legislation to repeal the SGR altogether.
Enter MACRA
With broad bipartisan support, the Medicare Access and CHIP Reauthorization Act (MACRA) passed the Senate 92–8 and the House 392–37. President Obama signed MACRA into law on April 16, 2015.[12] It did not simply leave Medicare providers free to bill the government fee-for-service as before. Instead, it sought a new approach to remedy the program’s tendency to foster the provision of ever-greater volumes of low-value services.
This problem has been a major concern since an influential 2001 report by the Institute of Medicine, which blasted the U.S. health-care system for inattention to quality, insufficient incentives for preventive care, poor coordination of providers, and voids of coverage in between services for which reimbursement was available.[13] Medicare’s payment structure—which reimburses physicians regardless of whether the patient is satisfied, correctly diagnosed, or provided with inappropriate and ineffective treatment—was greatly responsible for this situation.[14] A belief therefore grew that, since the unintended consequences of Medicare’s payment rules had engendered such dysfunction, reform should prod all clinicians to move in the right direction.
Title III of the Affordable Care Act made an initial step in this direction, by giving the executive branch much greater authority to develop new Medicare payment arrangements. MACRA expanded the scope of this power into a wholesale reform of physician payments, which would effectively eliminate the status quo as a viable option. With some justification, MACRA has been deemed “the most important federal legislation, to date, to impact health care delivery.”[15]
MACRA was the product of a bipartisan congressional compromise immediately motivated by a desire to fix SGR, partly motivated by the ideal of enhancing the value of the health-care system, and, to a large extent, constrained by a need to let sleeping dogs lie.
Few members of Congress paid much attention to the details of the bill, other than being glad to be rid of physician lobbyists pressing for a Doc Fix every year. A notable exception was Senator Ben Sasse (R., Neb.), who warned that the legislation “substitutes the flawed SGR formula for more than 120 pages of new rules to govern the practice of medicine.”[16] He was referring only to the statute. The final rule implementing the law for 2017 took up 824 triple-column pages of dense print in the Federal Register;[17] the proposed rule for 2018 was 491 pages more.[18]
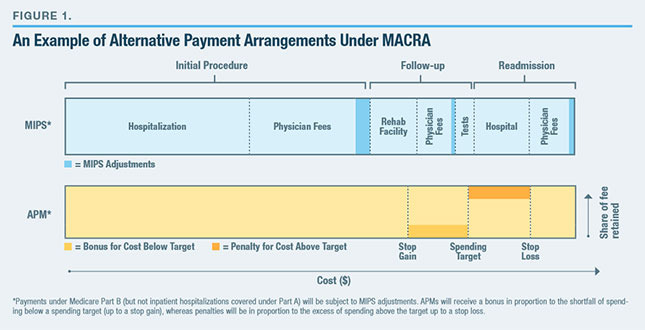
MACRA gives clinicians two options, which I have summarized in Figure 1: the Merit-based Incentive Payment System (MIPS), which adjusts Medicare’s fee-for-service reimbursement rates according to performance on an array of clinical practice metrics; and Advanced Alternative Payment Models (A-APMs), which reward or penalize practices according to how much their patients cost to treat relative to the medical care that federal rules estimate they need.
APMs are aggregated payment arrangements for a care episode, a course of treatment, or the full spectrum of Medicare services delivered to an individual patient. APMs are intended to encourage providers to care about patient outcomes, rather than simply render discrete services while rewarding them for reducing the total cost of services delivered. Such models establish financial incentives to develop cost-effective practice styles, reward activities taken that prevent complications, and promote both the development and take-up of new cost-saving technologies. This is designed to promote a well-coordinated care experience, which includes all services furnished during surgery, good follow-up care, and measures to minimize the risk of readmissions.[19] It is hoped that APMs would make clinicians responsible for ensuring high-quality care outcomes, without micromanaging how they achieve them.
MACRA advocates hope that MIPS will give smaller clinicians experience in outcome-based metrics needed for them to be willing to bear the financial risk associated with payments as APMs.[20]
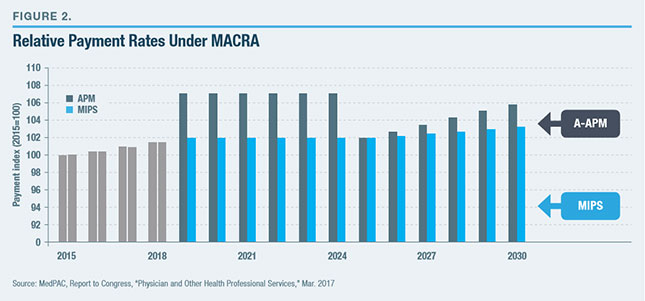
Payment updates are structured to encourage clinicians to shift from MIPS to APMs (Figure 2).[21] From 2019 to 2024, clinicians will be eligible for a 5% payment bonus if they qualify as A-APM providers by bearing “more than nominal risk,” whereas the rest would find their fee-for-service reimbursement rates subject to adjustment under MIPS. From 2026, A-APM qualified clinicians will receive annual payment increases of 0.75%, while those under MIPS will get increases of 0.25%.[22]
This, of course, assumes that Congress will not intervene with new legislation—an unlikely assumption, given the recent history of yearly legislation to alter Medicare physician fees.
The Method of MIPS

MIPS ranks clinicians relative to their peers (such as other oncologists, other nurse practitioners, or other speech pathologists) through an elaborate rating system—based on performance on a variety of metrics—which yields a composite score out of 100. Those meeting a threshold score, set by the Centers for Medicare & Medicaid Services (CMS), will qualify for an upward adjustment to their Medicare payment rates; those falling below will get a downward adjustment.

The adjustments will be calculated to be budget-neutral in the aggregate, so that the extent of the increase for clinicians scoring above the threshold will shrink as a larger share of their peers do so[23] (Figure 3). The maximum downward adjustment will be capped every year (rising to 9% from 2022), and political pressure can be expected to ensure that the threshold is set such that it is surpassed by a majority of clinicians—so upward adjustments may be spread very thin. For the first year, CMS set the threshold at three out of 100—a level so low that all entities reporting are expected to comply.[24] Bonus payments of $500 million per year for “exceptional performance” will also be added from 2019 to 2024 and shared by the top quartile of clinicians above the threshold.
MIPS adjustments will be based on clinicians’ performance two years prior—with scores first being used to adjust fees in 2019, based on activity in 2017.
MIPS, as an entity, was created by MACRA, but it is largely an amalgamation of physician payment rules established over the past decade. To reward physicians, performance scores aggregate metrics from four categories (Figure 4). On each metric, clinicians’ performance is compared with others from the same specialty.
The Madness of MIPS
Even though MIPS is still several years away from being fully implemented, MedPAC—the agency established by Congress to advise it on Medicare payment policy—has declared MIPS unworkable and called for it to be repealed.[27]
MedPAC has argued that MIPS imposes significant administrative costs on providers but cannot identify, let alone reward, value.[28] Even before MACRA, MedPAC warned: “Medicare’s current quality measurement approach is becoming ‘over-built,’ and is relying on too many clinical process measures that are, at best, weakly correlated with health outcomes.”[29] MedPAC commissioners deemed it likely that MIPS bonus payments would mostly reward statistical noise, suggested that its various metrics were a set of uncoordinated and arbitrary gestures, argued that “attestation only, ‘check the box’ sort of measures” would yield little but burdensome paperwork, and concluded that “it is extremely unlikely that clinicians will understand their score or what they need to do to improve it.”[30]
Quality Component
For instance, family physicians must choose six from among 38 different potential measures (i.e., out of 2,760,681 potential combinations of metrics) on which their performance is to be assessed. MedPAC uses these self-reporting data to grade them on a curve relative to other family physicians choosing the same measures.[31]
Success under such rules will likely measure the game-theoretic sophistication of clinicians in picking metrics that cause them to be compared with a relatively weak set of peers. It is hard to see how such an arrangement is likely to encourage cost-effective improvements in care. More likely, the greatest beneficiaries will be the vendors of software packages designed to help clinicians exploit the idiosyncrasies of the scoring system to their advantage.[32]
Given that providers may flock to metrics that are easiest to satisfy, slight disparities on the few metrics that are not topped out are likely to become enormously magnified. While this may allow the outcome-based metric chosen to dominate the array of meaningless process metrics, such an arrangement is likely to punish providers who treat the most difficult patients. This may deter physicians from treating the poor and seriously ill. Indeed, the inability to accurately identify and control for the impact of patient characteristics, which interact with a near-infinite variety of circumstances, makes it impossible for this method to properly hold physicians accountable for desired patient outcomes.
The U.S. Government Accountability Office has joined the growing chorus of criticism of MIPS and other physician payment rules, noting that “although hundreds of quality measures have been developed, relatively few are measures that payers, providers, and other stakeholders agree to adopt, because few are viewed as leading to meaningful improvements in quality.”[33]
Urban Institute fellow Robert Berenson has suggested that misdiagnosis (occurring in 5%–15% of cases) may be the prime medical quality challenge, but that this is unmeasured and unrewarded by MIPS.[34] Indeed, under fee-for-service, a provider may actually get more revenue if a patient is misdiagnosed and keeps coming back for treatment.
Resource Use Component
Brookings Institution scholar Niam Yaraghi has warned that providers have a long history of inflating self-reported measures and that the lack of any system for auditing or punishing misreporting means that MIPS is likely to exacerbate Medicare’s already-serious fraud problem.[35] The “resource use” component is the only element of MIPS calculated directly by CMS, rather than depending on the honor system to ensure accurate reporting.
But even if it were perfectly monitored, the penalty for excessive resource use will never weigh more than 30% as a component to a maximum potential 9% negative MIPS adjustment. Indeed, because this penalty is levied as a proportion of overall revenues, it may actually encourage physicians seeking to maintain the same overall income to inflate their volumes of office visits, lab tests, or scans.[36]
As with quality measures, the resource use metric fails to adequately adjust for the additional cost involved in treating patients with more complex medical needs. A recent study by Eric Roberts, Alan Zaslavsky, and Michael McWilliams found that exposure to the Value-Based Payment Modifier (the pre-MACRA penalty for overuse of resources) made no significant impact on the cost of care, but considerably reduced payments to practices serving a larger proportion of high-risk patients.[37]
CMS has attempted to mitigate this by supplementing total per-beneficiary measures of spending with per-episode ones, but this serves only to further dilute the impact of aggregate cost controls and to multiply the opportunities for manipulation of the system. Although bad actors have many ways to inflate volumes unnecessarily, honest clinicians simply have very little ability to control a beneficiary patient’s aggregate costs under an open-ended fee-for-service system.[38]
Access to Care Information Component
When the 2009 stimulus bill introduced a payment bonus for physician practices making “meaningful use” of Electronic Health Records, it could be justified as helping them defray up-front capital costs of transition to a new system during a recession. But these payments continue to be made every year, without generating clear improvements in care outcomes. Patients complain that physicians are too busy documenting interactions on laptops to properly listen to them, while data are usually stored away unused in systems that are rigid and rapidly obsolete and that fall well short of promised levels of interoperability.
Effective EHR technology should simplify physicians’ jobs, reduce duplicative paperwork, facilitate the communication of information, and help eliminate errors. If it is valuable, it should pay for itself by reducing costs. The EHR system established by the American Recovery and Reinvestment Act and entrenched by MACRA requires such substantial public subsidy because it is designed more for the purpose of extending bureaucratic control than it is for the sake of improving care.
Clinical Practice Improvement Activity Component
While the specific EHR activities that MACRA seeks to advance are loosely defined, the structure of its payments for Clinical Practice Improvement Activities possesses barely any unifying purpose at all. Its incentives seem to be modeled after the Boy Scouts’ merit badge system, with the intent of rewarding (on the honor system) whatever miscellaneous activities providers feel most inclined to engage in. Under this arrangement, the Eagle Scouts of the medical profession will be rewarded for surpassing their peers on public-spirited activities such as seeing new Medicaid patients in a timely manner, administering patient satisfaction surveys, and participating in new CMS payment initiatives.[39]
Overall Impact of MIPS
Needless to say, compliance with this regulatory scheme will be enormously costly. In 2017, the burden of MIPS reporting alone is estimated at $1 billion, and this can be expected to increase when physicians increasingly alter behavior and make investments to claim payment adjustments as MIPS is phased in.[40] Even high-scoring practices might find themselves losing out on balance.
One study estimated that physicians already spend, on average, 15 hours per week and a total of $15.4 billion per year dealing with Medicare’s existing quality measures.[41] This cost of compliance has been hardest for small medical practices to bear and has been one of the main forces driving consolidation into large medical systems. In small practices, statistical noise looms large in patient outcome data, so even those able to comply with regulatory mandates are likely to fare poorly under MIPS. CMS has estimated that 78% of practices with fewer than 10 staff (30% of clinicians) would get negative payment adjustments, while 81% of those with more than 100 employees (40% of clinicians) would enjoy positive adjustments.[42]
An arrangement whereby MACRA punishes practices whose solvency is already strained—small practices, those serving rural areas, and those serving the poor—is clearly politically unsustainable. To allay these concerns, CMS has created exemptions from MIPS (for new clinicians, those with low volumes of Medicare patients and those participating in APMs) so broad that more clinicians (800,000) will be exempt from the program in 2018 than participating (600,000).[43]
Physicians will not know what they have to do to qualify for payment bonuses, as the location of peer-based thresholds will be unknown to them ex-ante—potentially leading to great overinvestment in essentially pointless activities. The two-year time lag between performance and adjustment to payment rates will likely add further confusion. Political imperatives will necessarily distort the system over time, so that attempts to incorporate fairness shift metrics from rigid and objective criteria toward more politically malleable ones.
Rather than engaging in the near-impossible task of ranking every clinician fairly by attempting to account for every mitigating circumstance, MedPAC has suggested that quality regulation is likely to be ineffective beyond the modest task of punishing extreme poor performers or overutilizers.[44]
MIPS presumes patients and their families to be passive, rather than a force that can be mobilized as a free, incorruptible, and well-motivated monitoring agent, empowered to insist on quality through the choice of providers in the marketplace. Market forces will always be the primary mechanism for upholding quality: physicians offering poor services will lose patients to their competitors.
If additional regulatory protections are necessary for the sake of consumer protection or to ensure program integrity and the efficient use of taxpayer funds, these should be mandatory rather than optional activities, assessed only if providers wish to be assessed on those grounds. If some practice activities confer general benefits in terms of public health, each of these should be determined separately on its merits and the valuable ones purchased directly. Medicare should not be paying for physicians who fail to diagnose and deliver appropriate treatment, but marginal tweaks to payments within fee-for-service will not prevent that—especially if payments to clinicians continue to be increased in proportion to the volume of inputs employed, rather than defined relative to outputs for which they can be held accountable.
The APM Arrangement
By establishing payment increases for Qualifying APM Participants (QP) exceeding those under MIPS, Congress sought to nudge clinicians to opt for APMs. Practices must receive at least 25% of their Medicare revenue through an Advanced APM or receive payments for at least 20% of Medicare patients through an A-APM to gain QP status in 2019.[45] The 5% Medicare Part B reimbursement bonus for QP clinicians will not just apply to revenues received through A-APMs but also to revenues received by QPs for treating other patients fee-for-service.
From 2021, practices will have the option to count revenues from other payers (such as employer-sponsored insurance, Medicaid, Medicare Advantage, and other private insurance) to meet A-APM revenue thresholds. From 2023, clinicians must have at least 75% of all revenues (including 25% of Medicare payments) or 50% of patients (and 20% of Medicare payments) through an APM to maintain QP status.
To be counted as A-APMs that QPs can gain credit for enrolling in, payment models must:[46]
- Use Certified (Electronic Health Records) Technology (CEHRT)
- Report MIPS-like quality measures and base some payments on them
- Require payment risk exceeding 8% of benchmark levels, including potential losses exceeding 3%
The Actuality of APMs
The Obama administration set ambitious goals for shifting Medicare to APM arrangements and subsequently claimed credit for rapid increases in the number of participating organizations, improvements in the quality of care, and savings for taxpayers.[47] A more careful assessment makes clear that results fall well short of the hype.
While 1,986 organizations participated in six APM models in 2016, only 53 of these took part in two-sided risk models (including penalties as well as bonuses) involving the “more than nominal risk” needed to count as an A-APM.[48] The vast majority were what CMS calls “shared savings models” or “one-sided risk” arrangements (involving just bonuses). In theory, these would give providers an incentive to collaborate to reduce aggregate care costs, by allowing them to keep a portion of savings generated by reduced volumes. In reality, they impose no risk on providers at all, since clinicians can keep claiming reimbursement fee-for-service as before and can claim a bonus payment if their spending on assigned enrollees (for whatever reason, including luck or bureaucratic ignorance) was lower than expected by CMS.
Why would any provider group seek to reduce aggregate spending below that benchmark, to share savings with the government, if it can keep the full amount for itself by claiming reimbursement up to the full benchmark level—with no penalty if it goes above? Indeed, some providers could claim shared savings merely by continuing as before and claiming credit for random downward fluctuations in aggregate spending. As a result, the program in 2016 ended up costing CMS more money than was generated in savings.[49]
Ashish Jha of Harvard University noted that while 51.8% of shared savings organizations spent less than their target in 2015, 48.2% spent more—with those deemed to be “saving money” actually spending more than those deemed to be overspending, possibly because they had been judged against more generous benchmarks based on their own historically inflated spending levels.[50]
So that participation in APMs would not be limited to provider groups seeking to exploit overvalued benchmarks, the Obama administration proposed to make payment models with two-sided risk mandatory for cardiac rehabilitation, joint replacement, and some other care episodes. Unsurprisingly, providers have been less keen on an arrangement that might leave them worse off, so HHS secretary Tom Price (a former orthopedic surgeon) canceled three out of the four mandatory bundles soon after assuming office, while halving the number of regions subject to the other.[51]
There is a substantial risk of the costs of the Medicare program being inflated by “upcoding” if hospitals are able to claim payment for a full bundle whenever a patient seeks treatment at a hospital’s emergency department with an acute event linked to a covered condition.[52] Similarly, the availability of bundled payment arrangements also increases the need to police “unbundling”—to stop providers claiming reimbursement for the full bundle, while also continuing to bill for associated services separately as before.
This is the sort of challenge at which Medicare has traditionally failed miserably. In 2016, $41 billion (or 11%) of Medicare fee-for-service spending consisted of improper payments to providers—over $1,000 per beneficiary.[53] The desire to establish provider responsibility for the full spectrum of care is fundamentally at odds with an open-ended fee-for-service benefit structure hardwired to make it easy for any beneficiaries to receive as many services as they wish from any provider anywhere.
While a desire to expand DRGs into fuller bundles makes sense, more ambitious attempts to re-create elements of managed care within Medicare’s fee-for-service reimbursement will necessarily be hobbled because of the inability of provider groups to prevent beneficiaries from consuming low-value services elsewhere.[54] Indeed, even APMs with two-sided risk arrangements have neither the proper incentive nor the ability to fully reward beneficiaries to refrain from doing so.
What to Make of MACRA?
A 2016 survey of medical groups by the Advisory Board, a health-care consultancy, found 70% of respondents “concerned” or “totally freaked out” by MACRA, with only 20% “confident” and 10% “ambivalent.”[55] Yet it is fair to imagine that MACRA’s twin-track structure will form the basis of any further reforms that are made, and its merits and flaws deserve to be examined.
John O’Shea of the Heritage Foundation has suggested that MACRA seeks to shift the health-care delivery system toward value-based payment “by making FFS [fee-for-service] increasing[ly] unattractive, while simultaneously developing and implementing APMs for providers to transition into.”[56] But he warns that “MIPS will make FFS untenable at a much faster pace than the development and implementation of viable APMs.”[57]
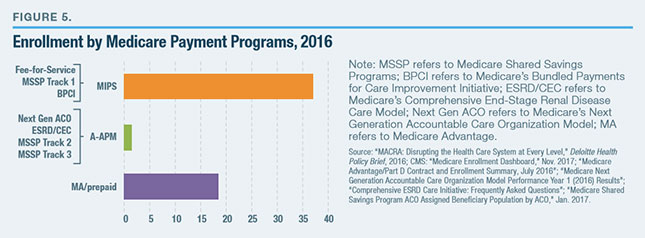 It is hard to imagine that Congress would sit idle, while the vast majority of Medicare beneficiaries and clinicians are trapped in an unviable fee-for-service system (Figure 5). Many of the regulatory requirements imposed under MIPS apply specifically to APMs, too. Although current law intends payments for APMs to become more attractive than those for MIPS over time, it is quite likely that MIPS will soon get patched, as SGR was in the past.
It is hard to imagine that Congress would sit idle, while the vast majority of Medicare beneficiaries and clinicians are trapped in an unviable fee-for-service system (Figure 5). Many of the regulatory requirements imposed under MIPS apply specifically to APMs, too. Although current law intends payments for APMs to become more attractive than those for MIPS over time, it is quite likely that MIPS will soon get patched, as SGR was in the past.
This is particularly true, given that the feasibility and availability of APMs are likely to vary inequitably by medical specialties and practice locations. There are, for instance, currently no APMs available for emergency physicians, and their establishment is likely to be considerably more difficult in rural areas.
APMs represent a difficult challenge for small practices, which lack the patient numbers necessary to spread risks that they would be required to assume. While it has been suggested that multiple small practices could pool risks, this necessarily creates another layer of moral hazard, and small practices already lack the administrative capacity to coordinate and manage the full spectrum of services needed by patients under APMs. Regulations have exacerbated this natural disadvantage faced by small independent practices by requiring all payment bundles to be anchored by an inpatient hospital—preventing specialty clinics and surgery centers from capitalizing on their ability to deliver an often-superior product at much lower cost.[58]
This has fueled concerns that MACRA could drive the further consolidation of American health care. Some 67% of Medicare-dependent practices with five or fewer staff see MACRA as ending their independence, while 89% say that they will reduce Medicare volumes in an attempt to remain exempt.[59] The proportion of physicians in independent practice has already declined rapidly, from 49% in 2012 to 33% in 2016.[60]
Kathleen Sebelius, secretary of Health and Human Services under President Obama, admitted that APMs were in “constant tension” with antitrust law.[61] Scott Gottlieb of the American Enterprise Institute, since appointed commissioner of the Food and Drug Administration by President Trump, warned that MACRA threatened “a permanent end to the private practice of medicine,” by forcing doctors into salaried appointments by large hospital monopolies, with every element of care micromanaged and rationed by government bureaucrats.[62] Yet in practice, APMs have been so ineffective that there is little evidence that they have made a significant contribution to the consolidation that is currently occurring.[63]
A Better Way Forward
MACRA has two core goals: replacing SGR’s failed method of fixing Medicare’s volume problem; and using the Medicare program to reduce the provision of unnecessary or low-value care more generally. The first goal is a big enough challenge, and successfully addressing it would achieve much of the second objective.
MIPS should be repealed and the quality of medical care enhanced by strengthening simpler mechanisms. Patients have the strongest interest in the quality of care, and Medicare should instead strengthen their ability to shop for it. Furthermore, the program should simply refuse to pay providers where misdiagnosis or mistreatment can be identified.
Prospective payment has served well in empowering consumers and increasing efficiency in the delivery of hospital care. The use of APMs to expand such payment bundles by incorporating physician fees and other services is clearly desirable—but voluntary or retrospective shared savings arrangements will do little to advance either objective.
Policymakers have long lamented that Medicare’s traditional fee-for-service structures reward providers for adopting costly medical practice styles and billing for an inordinate volume of inappropriate tests and other services. But when a Medicare beneficiary chooses a Medicare Advantage (MA) plan, the exposure of taxpayers to costs driven by inflated volumes of unnecessary or low-value care is entirely capped.
When an individual chooses a Medicare Advantage plan, the plan receives a single payment, adjusted according to enrollees’ expected medical needs, to provide the full spectrum of Medicare-covered services. This payment structure encourages plans to provide the most effective care at the lowest cost. This is true even if that individual opts for a Private Fee-for-Service (PFFS) Medicare Advantage plan rather than a Managed Care MA plan with gatekeeping or tiered cost-sharing to encourage the use of in-network providers. Indeed, the 100% two-sided risk adopted by PFFS MA plans is more of a complete solution to the alignment of incentives to solve Medicare’s cost problem than MACRA’S most ambitious A-APM.
The Obama administration refused to give clinicians credit for beneficiaries enrolled in MA plans for the sake of meeting their target of Medicare patients enrolled in APMs needed to gain QP status and the associated reimbursement bonus. The Trump administration has since established a payment demonstration, so that APM contracts within MA plans may be counted to this end.[64] But this may serve more to ensnare MA plans into acting as enforcers for MIPS regulations tied to APM rules than it does to prevent inflated volumes of low-value care.
Given that enrollment of Medicare beneficiaries in any kind of MA plan is sufficient to eliminate the incentive for ever-inflated volumes, beneficiaries from any MA plan should be counted toward a participating clinician’s or medical practice’s QP status. This change might be implemented by executive action.
It has been repeatedly demonstrated that enrollment in MA managed-care plans yields significant spillover gains for non-enrollees, by promoting cost-effective practice styles.[65] Yet looser MA networks are the genuine on-ramp to effective value-based care through MA that others have imagined MIPS to be. Indeed, being paid by capitation, all MA plans are subject to systematic incentives in favor of delivery-system transformation in the long run. Widely celebrated integrated systems, such as Geisinger or Kaiser, are already able to do everything they need within MA. That payment environment provides the incentives and freedom that others need to emulate so they can save money and generate better care outcomes but without forcing them to do so where it does not.
Medicare has a tough enough job delivering cost-effective quality care for its beneficiaries. The fact that it has inadvertently shaped the health-care delivery system, by impeding competition and inflating costs for other payers, does not mean that it is capable of serving as a tool for micromanaging the entire health-care delivery system—in fact, it suggests quite the opposite.
By aligning incentives more appropriately, Medicare Advantage is a much better tool for advancing fundamental reform. By allowing providers a way to escape the madness of MIPS, it might be essential to clinicians in the shorter run, too.
Endnotes
- Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2017 Annual Report, July 13, 2017.
- “Implementing MACRA,” Health Affairs Policy Brief, Mar. 27, 2017.
- Office of Inspector General, U.S. Department of Health & Human Services, “Medicare Hospital Prospective Payment System: How DRG Rates Are Calculated and Updated,” OEI-09-00-00200, Aug. 2001.
- Ibid.
- Centers for Medicare & Medicaid Services (CMS), “National Health Expenditures.”
- Charles Roehrig, “A Brief History of Health Spending Since 1965,” Health Affairs blog, Sept. 19, 2011.
- American Medical Association, “RBRVS Overview.”
- Congressional Budget Office (CBO), “Factors Underlying the Growth in Medicare’s Spending for Physicians’ Services,” Background Paper #2597, June 2007.
- Zirui Song et al., “Medicare Fee Cuts and Cardiologist-Hospital Integration,” JAMA Internal Medicine 175, no. 7 (July 2015): 1229–31.
- Medicare Payment Advisory Commission (MedPAC), Report to Congress, “Physician and Other Health Professional Services,” Mar. 2017.
- “Implementing MACRA.”
- Medicare Access and CHIP Reauthorization Act of 2015, Public Law 114-10.
- Institute of Medicine, “Crossing the Quality Chasm: A New Health System for the 21st Century,” Mar. 2001.
- Chris Pope, “Medicare’s Single-Payer Experience,” National Affairs, no. 26 (Winter 2016): 2–20.
- Kathryn Toone, Natalie Burton, and David Muhlestein, “MACRA in 2017: Overview, Impact & Strategic Considerations of the Quality Payment Program,” Leavitt Partners, Mar. 2017.
- Ben Sasse, “House Should Reject Medicare Change,” Politico, Mar. 26, 2015.
- CMS, “Medicare Program; Merit-Based Incentive Payment System (MIPS) and Alternative Payment Model (APM) Incentive Under the Physician Fee Schedule, and Criteria for Physician Focused Payment Models,” Final Rule with comment period, Federal Register 81, no. 214 (Nov. 4, 2016): 77008–831.
- CMS, “Medicare Program; CY 2018 Updates to the Quality Payment Program,” Proposed Rule, Federal Register 82, no. 125 (June 30, 2017): 30010–500.
- Tim Gronniger et al., “How Should the Trump Administration Handle Medicare’s New Bundled Payment Programs?” Health Affairs blog, Apr. 10, 2017.
- Toone, Burton, and Muhlestein, “MACRA in 2017.”
- CMS, “The Quality Payment Program.”
- MedPAC, Report to Congress, “Physician and Other Health Professional Services,” Mar. 2017.
- CMS, “The Merit-Based Incentive Payment System: MIPS Scoring Methodology Overview.”
- MedPAC, Report to Congress, “Medicare and the Health Care Delivery System,” June 2017.
- MedPAC, “Physician and Other Health Professional Services.”
- Eric T. Roberts, Alan M. Zaslavsky, and Michael McWilliams, “The Value-Based Payment Modifier: Program Outcomes and Implications for Disparities,” Annals of Internal Medicine 168, no. 4 (Nov. 28, 2017): 255-65.
- See the transcript of the MedPAC public meeting, Oct. 5, 2017, pp. 4, 9; Virgil Dickson, “MedPAC Urges Repealing MIPS,” Modern Healthcare, Oct. 5, 2017.
- Kate Bloniarz and David Glass, “Next Steps for the Merit-based Incentive Payment System (MIPS),” MedPAC public report, Oct. 5, 2017.
- See the letter from Glenn M. Hackbarth, chairman of MedPAC, to Marilyn Tavenner, administrator, Centers for Medicare & Medicaid Services, “RE: CMS List of Measures Under Consideration for December 1, 2014,” Jan. 5, 2015.
- See the transcript of the MedPAC public meeting, Oct. 5, 2017, p. 7.
- Niam Yaraghi, “MACRA Proposed Rule Creates More Problems than It Solves,” Health Affairs blog, Oct. 16, 2016.
- “MIPS Reporting Solutions,” Philips wellcentive; “MIPS Registry,” pMD.
- U.S. Government Accountability Office, “HHS Should Set Priorities and Comprehensively Plan Its Efforts to Better Align Health Quality Measures,” Report to Congressional Committees, GAO-17-5, Oct. 2016.
- Robert A. Berenson, “If You Can’t Measure Performance, Can You Improve It?” Journal of the American Medical Association 315, no. 7 (Feb. 16, 2016): 645–46.
- Yaraghi, “MACRA Proposed Rule.”
- J. Michael McWilliams, “MACRA: Big Fix or Big Problem?” Annals of Internal Medicine 167, no. 2 (July 18, 2017): 122–24.
- Roberts, Zaslavsky, and McWilliams, “The Value-Based Payment Modifier.”
- Lynn Bar, Tim Gronniger, and Tim Putnam, “CMS’s Big MACRA Surprise—Physicians Will Be Judged Based on Cost in 2018 MIPS Calculation,” Health Affairs blog, Nov. 22, 2017.
- Krista Teske, “Your Questions About the 2017 MACRA Final Rule—Answered,” Advisory Board Expert Insight, Jan. 31, 2017.
- Bloniarz and Glass, “Next Steps for the Merit-Based Incentive Payment System (MIPS).”
- Lawrence P. Casalino et al., “US Physician Practices Spend More than $15.4 Billion Annually to Report Quality Measures,” Health Affairs 35, no. 3 (Mar. 2016): 401–6.
- “Table 64: MIPS Proposed Rule Estimate Impact on Total Allowed Charges by Practice Size,” Federal Register 81, no. 89 (May 9, 2016): 28375.
- See the transcript of the Med PAC public meeting, Oct. 5, 2017.
- Kate Bloniarz and David Glass, “Approaches to MACRA implementation: Balancing MIPS and A-APMs,” MedPAC presentation, Jan. 12, 2017.
- Toone, Burton, and Muhlestein, “MACRA in 2017.”
- Tara O’Neill Hayes, “Primer: MACRA and Advanced Alternative Payment Models,” American Action Forum, Mar. 30, 2017.
- CMS, “Physicians and Health Care Providers Continue to Improve Quality of Care, Lower Costs,” Aug. 25, 2016.
- “MACRA: Disrupting the Health Care System at Every Level,” Deloitte Health Policy Brief, 2016.
- Maria Castellucci, “CMS Loses Money as Medicare ACOs Remain Risk-Averse,” Modern Healthcare, Nov. 3, 2017.
- Ashish Jha, “ACO Winners and Losers: A Quick Take,” An Ounce of Evidence blog, Aug. 30, 2016.
- Kristen Barlow, “3 Mandatory Bundles Will Likely Be Canceled, a 4th Scaled Back: What You Need to Know,” Advisory Board at the Helm, Aug. 16, 2017.
- François de Brantes, “Medicare’s Bundled Payment Programs Suffer from Fatal Flaws, but There Is a Logical Alternative,” Health Affairs blog, May 9, 2017.
- CMS, “Medicare Fee-for-Service 2016 Improper Payments Report.”
- J. Michael McWilliams et al., “Outpatient Care Patterns and Organizational Accountability in Medicare,” JAMA Internal Medicine 174, no. 6 (June 2014): 938–45.
- Yena Son and Daniel Kuzmanovich, “Concerned About MACRA? You’re Not the Only One,” Advisory Board Practice Notes, Dec. 8, 2016.
- John O’Shea, “Salvaging MACRA Implementation Through Medicare Advantage,” Health Affairs blog, Oct. 16, 2017.
- Idem, “As MACRA Implementation Proceeds, Changes Are Needed,” Health Affairs blog, Apr. 21, 2017.
- De Brantes, “Medicare’s Bundled Payment Programs Suffer from Fatal Flaws.”
- “Physicians Wary of MACRA’s Potential to Hasten the Demise of Independent Practices, per Black Book Survey,” PR Newswire, June 13, 2016.
- “2016 Survey of America’s Physicians,” Physicians Foundation, Sept. 21, 2016.
- Molly Gamble, “Sebelius: PPACA, Antitrust Law in ‘Constant Tension,’ ” Becker’s Hospital Review, Apr. 9, 2013.
- Scott Gottlieb, “House Republicans Should Break the Obamacare Mold on Doctor Pay,” Forbes, Mar. 19, 2015.
- Hannah T. Neprash, Michael E. Chernew, and J. Michael McWilliams, “Little Evidence Exists to Support the Expectation That Providers Would Consolidate to Enter New Payment Models,” Health Affairs 36, no. 22 (Feb. 2017): 346-54.
- “CMS to Count Participation in MA Towards Alternative Pay Model Calculations,” Inside Health Policy, Nov. 8, 2017.
- Katherine Baicker, Michael E. Chernew, and Jacob E. Robbins, “The Spillover Effects of Medicare Managed Care: Medicare Advantage and Hospital Utilization,” Journal of Health Economics 32, no. 6 (Dec. 2013): 1289–1300; Katherine Baicker and Jacob A. Robbins, “Medicare Payments and System-Level Health-Care Use: The Spillover Effects of Medicare Managed Care,” American Journal of Health Economics 1, no. 4 (Fall 2015): 399–431.
Photo: Valeriya / iStock / Getty Images Plus
Are you interested in supporting the Manhattan Institute’s public-interest research and journalism? As a 501(c)(3) nonprofit, donations in support of MI and its scholars’ work are fully tax-deductible as provided by law (EIN #13-2912529).